Healthcare deals with massive data sets, but most systems still don’t talk to each other.
Different hospitals, labs, and clinics often speak entirely different languages in terms of tech. So, when one system needs to communicate with another to obtain the desired data, things become complicated.
Enter interoperability. It essentially means getting healthcare systems, old and new, to share data (such as patient records) in ways that are safe, standardized, and actually useful.
You’ve probably heard of HL7 and FHIR. However, what do these standards do? And how do you know which one to work with?
This article discusses the major healthcare interoperability standards, such as HL7, FHIR, and more. You’ll learn what they’re built for, where they’re used, and how to deal with them when building or scaling your own HealthTech product.
What Is HL7? And Why Should You Care?
HL7 stands for Health Level Seven and is one of the oldest and most widely used standards in healthcare. It’s a set of rules that help different healthcare systems exchange data, especially in hospitals.
If you’ve ever built software that needs to talk to an electronic health record (EHR), lab system, or billing tool, there’s a good chance HL7 is in the mix.
There are two major versions you’ll run into:
- HL7 v2: The workhorse. Used everywhere. Sends messages like lab results, patient admissions, discharge summaries, and billing updates. It’s text-based, a bit cryptic, but it gets the job done.
- HL7 v3: An attempt to modernize things with XML and a stricter model. It didn’t gain much traction outside a few regions, so most systems still stick with v2.
HL7 v2 is often what connects your app to legacy systems. Labs, hospitals, and insurance providers all still run on it. So, HL7 is a very likely part of your integration stack.
What Is FHIR (Fast Healthcare Interoperability Resources)?
FHIR (pronounced “fire”) is the newer, web-friendly standard that’s quickly becoming the go-to choice for modern HealthTech apps. HL7 developed it, but unlike its older sibling (HL7 v2), FHIR actually seems like it was made for developers.
The FHIR standard is built on web technologies like REST APIs, JSON, and OAuth2. So, if you’ve worked with any modern API, you’ll feel right at home. It focuses on clean endpoints and predictable responses, unlike cryptic pipes and carets as with HL7 v2.
It organizes health data into "resources", or modular pieces like:
- Patient (basic demographics)
- Observation (lab results, vitals)
- Encounter (a visit to the clinic)
- Condition, AllergyIntolerance, MedicationRequest, and many more
You can combine these to build custom workflows. Want to pull a patient’s vitals from an EMR? Need to share discharge summaries between systems? FHIR is the way to go.
Big names like Epic, Cerner, Apple Health, and Google Cloud Healthcare API already support FHIR. If you're exploring modern development stacks, here’s a curated list of the top healthcare APIs for advanced apps that can help you integrate securely, efficiently, and at scale.
So, if you’re building anything new in healthcare, start with FHIR. Seriously. It saves time, makes integration smoother, and is already becoming the industry standard.
Other Important Standards (and When to Use Them)
FHIR and HL7 are popular, but they’re not the only ones you’ll run into.
Here are a few others that show up often in real-world projects:
CDA (Clinical Document Architecture)
CDA helps send long-form documents like discharge summaries or referrals. It’s XML-based and still used in older systems.
Use it when you're dealing with legacy EHRs or documentation-heavy workflows.
DICOM (Digital Imaging and Communications in Medicine)
DICOM handles medical images such as MRIs and X-rays. It also includes patient information with each image.
Use it for radiology tools, image viewers, or AI that works with scans.
LOINC, SNOMED CT, and ICD
These are vocabularies that help make clinical data consistent.
LOINC is for lab tests and results. SNOMED CT covers medical terms and conditions. ICD is used for diagnoses and billing codes.
Use them to keep your data clean, especially for analytics, reporting, or insurance workflows.
IHE (Integrating the Healthcare Enterprise)
IHE is a framework that shows how different standards should work together. It helps different systems communicate smoothly.
Use it when you're connecting tools across vendors or health systems.
TEFCA (Trusted Exchange Framework and Common Agreement)
TEFCA is a U.S. policy for nationwide health data sharing. It defines how networks connect and build trust.
Use it if you work with U.S. providers or plan to join a national data exchange.
ISO Standards in Healthcare
ISO publishes global standards for health data security, quality, and compliance.
Use them in regulated fields like diagnostics, medical devices, or digital health that serve global markets.
In real-world apps, you’ll rarely use just one of these. Most big teams juggle a few: FHIR for real-time APIs, HL7 v2 for legacy messaging, DICOM for imaging, and vocabularies like LOINC or SNOMED CT behind the scenes.
The Four Levels of Interoperability in Healthcare
Interoperability isn’t the same as wiring two HealthTech systems together. It happens in layers.
Check out the four core levels of interoperability, from the basics to full-blown collaboration.
1. Foundational Interoperability
At this level, systems can exchange data, but they don’t really understand it.
For instance, a hospital faxes or uploads a discharge summary PDF to another clinic’s portal.
2. Structural Interoperability
Now the data has structure. Systems can identify specific fields like names, dates, or lab values.
For example, a lab sends results in HL7 or FHIR, and the receiving system maps them into the patient’s record.
3. Semantic Interoperability
Here’s where the systems actually understand the meaning behind the data.
For instance, a diagnosis coded using SNOMED CT or ICD, making it possible to trigger decision support or analytics across platforms.
4. Organizational Interoperability
This level is about policies, governance, and workflows, not just tech. It's what makes cross-org data sharing actually work in practice.
For example, providers exchanging data through TEFCA or multiple hospitals syncing data via a regional HIE.
Understanding these levels helps you plan better integrations and figure out where your system stands today.
Real-World Interoperability: What Does It Look Like in Practice?
Here are a few common real-world scenarios to visualize the importance of interoperability.
1. A Clinic Pulls Patient Data from a Hospital EHR
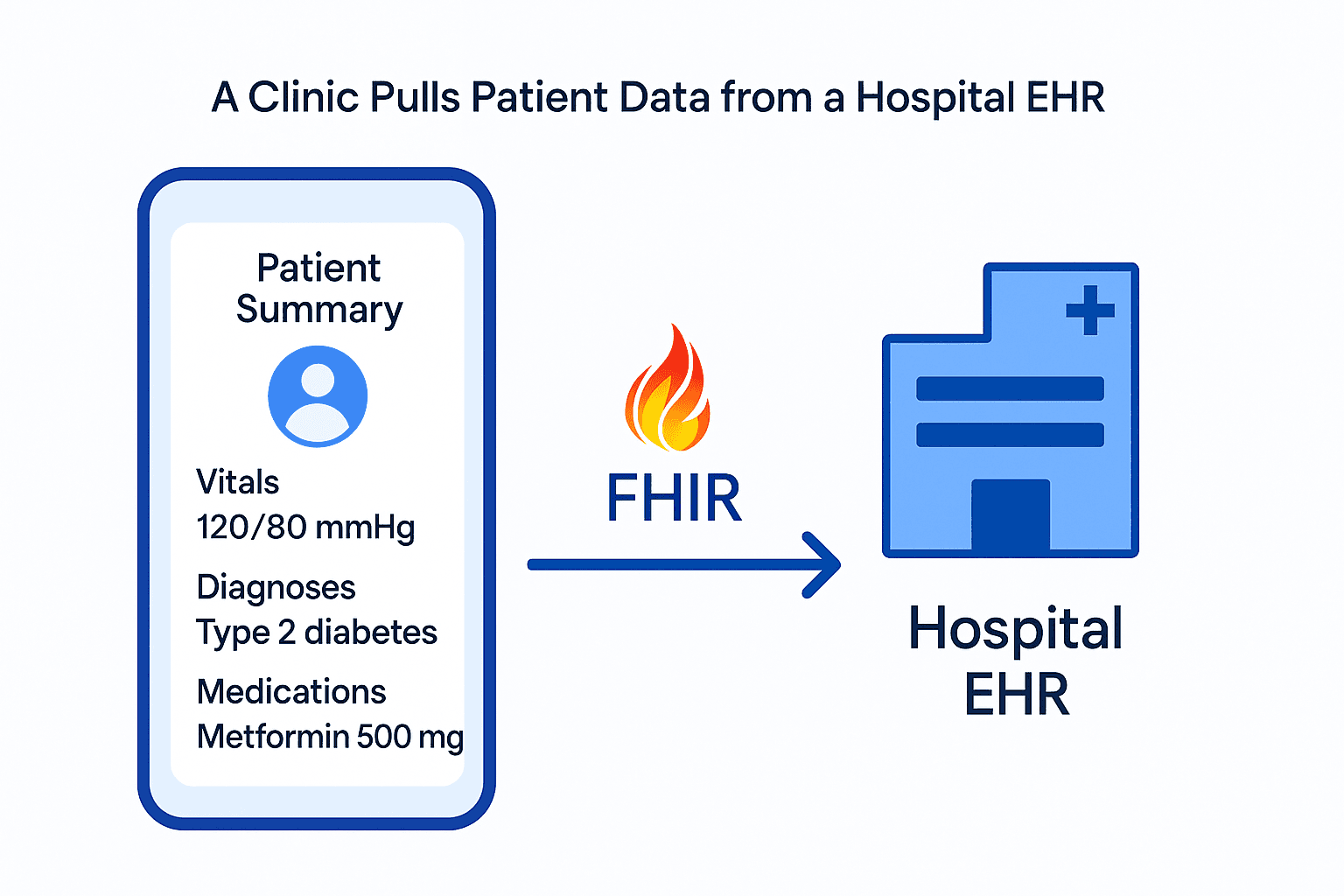
A digital health app wants to show a patient’s latest vitals, diagnoses, and meds.
The app uses FHIR APIs to connect with the hospital’s EHR (like Epic or Cerner). It pulls Patient, Observation, and MedicationRequest resources in JSON. SMART on FHIR, OAuth2, and a bunch of privacy rules working behind the scenes are what make it possible.
2. A Lab Sends Test Results to a Primary Care Doctor
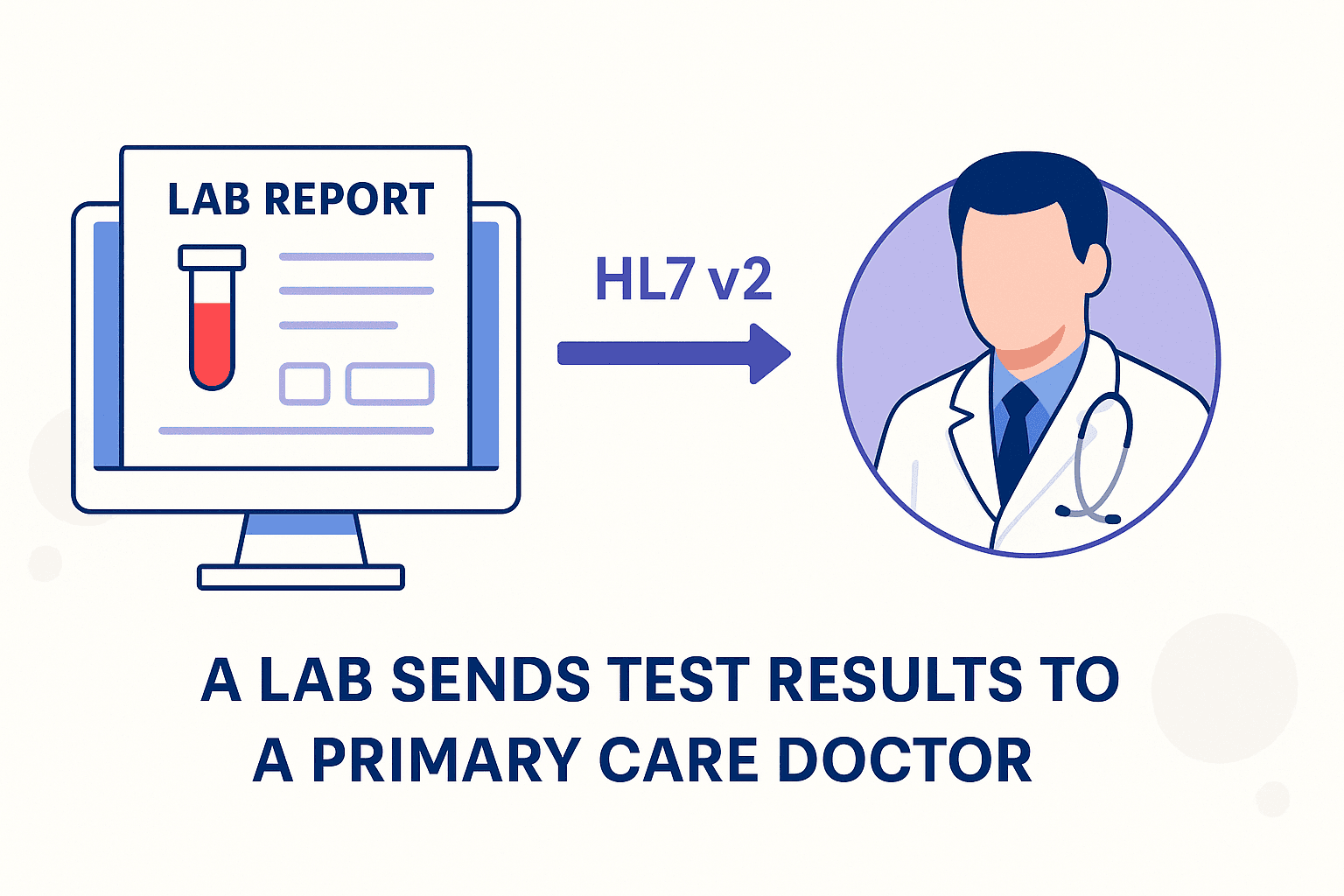
A lab completes a blood panel and sends the results to the clinic that ordered it.
The lab uses HL7 v2 messaging (like an ORU^R01 message) to push results to the clinic’s EHR. In this case, the old-school HL7, secure messaging protocols, and some IT duct tape help this happen.
3. A National Health System Standardizes Coding
Different clinics use different EMR and EHR systems. Even so, they all use the same codes for diagnosis and labs.
That is, everyone codes diagnoses using ICD-10 and lab tests using LOINC. Semantic interoperability, shared vocabulary, is how you can then search, aggregate, and analyze the data system-wide.
4. A Startup Connects to Multiple Systems with One API
Instead of integrating with every EHR separately, a healthtech startup uses a middle layer.
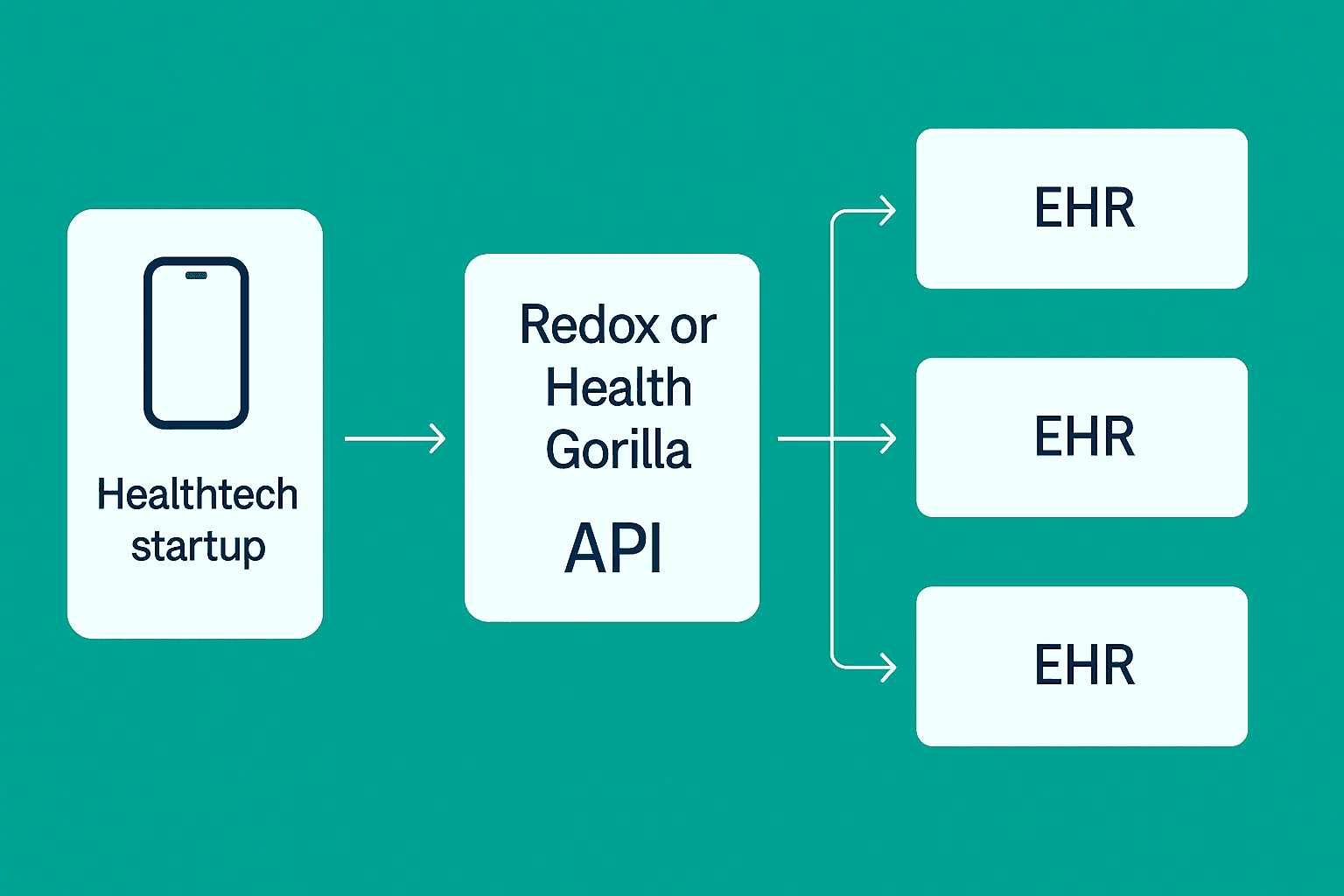
The app connects to Redox or Health Gorilla. Those platforms handle the messy HL7/FHIR translations and talk to different EHRs behind the scenes. So, an API middleware, standardization layers, and a whole lot of thoughtful abstraction are what allow the startup to connect various systems in an easy way.
Long story short, modern healthcare apps juggle old and new standards to keep data moving safely and meaningfully.
Challenges You’ll Face (and How to Solve Them)
Interoperability comes with a few headaches. Here are the common ones and how to deal with them.
1. Legacy Systems
A lot of healthcare infrastructure is still running on 20+ year-old tech. You might be using FHIR in your app, but the hospital you’re integrating with is still pushing out HL7 v2 messages from a mainframe.
To tackle this, use integration platforms like Redox, Health Gorilla, or 1upHealth to bridge the gap. They handle the old formats and give you cleaner, modern APIs.
2. Data Mapping and Inconsistencies
One system calls it “Sodium.” Another logs it as “Na+.” Some use LOINC codes. Some don’t use codes at all. You get the idea.
For this, use standard vocabularies like LOINC, SNOMED CT, and RxNorm wherever possible. And build a strong data normalization layer into your pipeline.
3. Privacy, Consent, and Compliance
Healthcare data is heavily protected. However, navigating HIPAA, GDPR, and other regional rules can slow development and kill momentum.
So, bake compliance into your architecture early. Use OAuth2, audit logs, token-based access, and encrypted data storage. If you're using the FHIR standard, look into SMART on FHIR for a standards-based approach to secure access.
4. Vendor Lock-in
Some vendors claim to be “FHIR-compliant,” but limit what data you can actually access or charge steep fees for integrations.
To avoid issues later on, ask the hard questions up front. Get clarity on which FHIR resources are available, how updates work, and what kind of support you’ll get during implementation. Always build with future migration in mind.
Tackle Healthcare Interoperability Easily With SoluteLabs!
Interoperability in healthcare can sound complex.
Start by understanding the standards, knowing what each one’s good at, and being realistic about what systems you’re connecting to. FHIR might be the future, but HL7, DICOM, and CDA are still running the show in a lot of places. Your app needs to speak both old and new.
Fortunately, with the right architecture and the right partner like SoluteLabs, you can build HealthTech products that work across systems, protect patient data, and scale as the industry evolves.
Planning to build or modernize a healthcare product? Let’s talk.
